What Are Bedsores?
A bedsore is a wound that forms when excess pressure is placed on the skin. This prevents blood flow from reaching the skin and causes skin cells to die.
Bedsores typically start as red or purple marks on the skin. If the bedsore goes untreated, it can break the skin and cause an open wound. The most serious bedsores burrow deep into the skin and expose bone, putting the victim at risk of life-threatening infections.
Bedsores are a common nursing home injury. Residents of long-term care facilities are at a greater risk of nursing home bedsores if they have handicaps that limit their movement. Since they can’t move properly, they may sit or lie in the same spot for hours and cut off blood flow to their skin.
Nursing home staff members should be able to prevent bedsores in these residents — but this doesn’t always happen. Every year, older adults develop deadly bedsores while staying in facilities that are supposed to take proper care of them.
Thankfully, there is help for those who suffered from bedsores due to nursing home neglect or abuse. Legal action can award victims with financial compensation for treatments and hold the nursing home staff accountable for their negligence.
What Causes Bedsores in Nursing Homes?
The main cause of bedsores is a loss of blood flow to the skin for an extended span of time. Blood flow can easily get cut off to the skin if nursing home residents are not mobile and sit or lie in the same spot for too long.
Causes of a lack of mobility include the following:
- Coma
- Injuries that require bed rest/wheelchair use
- Paralysis
- Poor health
- Sedation
- Surgical recovery


According to the Mayo Clinic, there are three main forces that can lead to bedsores in nursing homes.
- FrictionFriction occurs when the skin is dragged against another surface. For example, a patient’s skin may be pulled across the bed during position changes.
- PressureThis force can cause damage when the pressure of the skin against an object is greater than the pressure inside the body’s blood vessels. This damages and kills skin tissue.
- ShearShear is similar to friction but happens when two surfaces move in different directions. Shear can occur when the skin itself moves but the bones and muscle underneath stay in the same place.
Nursing home bedsores are more common in bony areas of the body like the tailbone, ankles, and heels. They tend to develop in places on the body that aren’t padded with muscle or fat.
Nursing Home Bedsore Risk Factors
Those who are at a greater risk of bedsores have limited mobility and may remain in bed or a wheelchair for long periods of time. Several factors can increase the risk of bedsores among vulnerable nursing home residents.
Age
Older individuals may have skin that is thin, fragile, dry, and less elastic than younger people. This makes it easier for a nursing home bedsore to develop.
Health
Many health problems can cause someone to develop a nursing home bedsore.
Medical conditions that make bedsores more likely include:
- Alzheimer’s or DementiaThese mental impairments can make it hard for residents to know when it’s time to reposition themselves. It can also prevent the resident from asking for help if they’re uncomfortable or in pain.
- Diseases That Decrease Blood FlowIllnesses like diabetes and vascular disease can decrease blood flow to the skin. Residents with these conditions have a higher risk of developing bedsores if they are not properly taken care of.
- IncontinenceIf the skin is excessively moist due to incontinence, it can increase the friction between clothing, beds, and the skin. People with bowel incontinence can also get local infections of the buttocks which can spread to nursing home bedsores.
- Muscle SpasmsPeople with muscle spasms have a higher risk of shearing their skin against a bed or wheelchair.
- Poor Nutrition and HydrationThose who lose weight due to malnutrition will lose protective fat below the skin, making them more prone to nursing home bedsores. Further, those who are dehydrated or have poor nutrition will need more time to recover from a bedsore.
- SmokingSmoking allows a lot of toxic chemicals to invade the body. These can restrict blood flow and hinder healing. The American College of Surgeons encourages anyone with a pressure ulcer to stop smoking.
- Spinal Cord InjuriesThose with spinal cord injuries or other neurological disorders that cause them to lack independent mobility can develop nursing home bedsores if they are not moved frequently.
Symptoms of Bedsores
The symptoms of bedsores are mild at first and gradually worsen as the wound tunnels into the body.
In the early stages of a bedsore, there won’t be an open wound. Instead, the skin will be discolored (typically red or purple) and the affected area will be painful to touch. Nursing home bedsores in this stage may also feel hotter or colder than normal skin.
An open wound will appear if the bedsore is not quickly treated. As the nursing home bedsore worsens, pus and blood may leak from it. The skin can turn black as necrosis (the death of healthy tissue) occurs.
Severe nursing home bedsores reach down deep into underlying tissue and can even expose bone. These bedsores put older adults at a high risk of infections – which can even be fatal.
See if you can work with a legal professional after a bedsore forms. Get a free case review.
Nursing Home Residents at Risk of Bedsores
Unfortunately, bedsores are quite common and very dangerous. The Agency for Healthcare Research and Quality (AHRQ) found that over 2.5 million people in the United States develop bedsores every year.
Any nursing home resident can develop a bedsore if they don’t reposition themselves regularly. People with medical problems that prevent them from turning themselves in bed or in a wheelchair are at the highest risk of developing bedsores.
Wheelchair-Bound Residents
For nursing home patients confined to wheelchairs, nursing home bedsores usually occur on bony areas of the body.
These include the:
- Backs of the arms and legs
- Buttocks
- Shoulder blades
- Spine
- Tailbone
Bedridden Residents
For elderly patients who are bedridden, nursing home bedsores form in slightly different areas than those who are wheelchair-bound.
These areas are the:
- Ankles
- Back of the head
- Back of the knees
- Ears
- Heels
- Hip
- Lower back
- Shoulder blades
- Tailbone
Stages of Nursing Home Bedsores
There are various stages of bedsores that differ in severity. Leading medical organizations like the Centers for Disease Control and Prevention (CDC) and the Mayo Clinic break down bedsores into four stages.
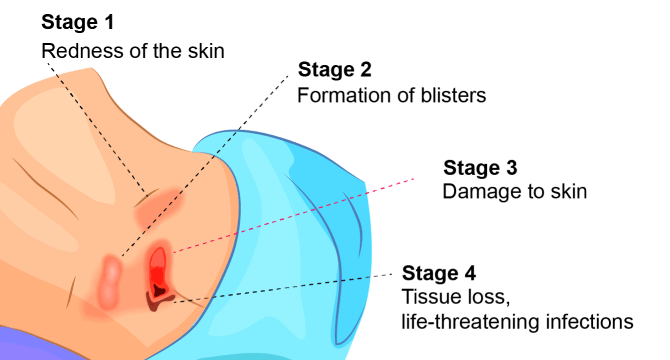
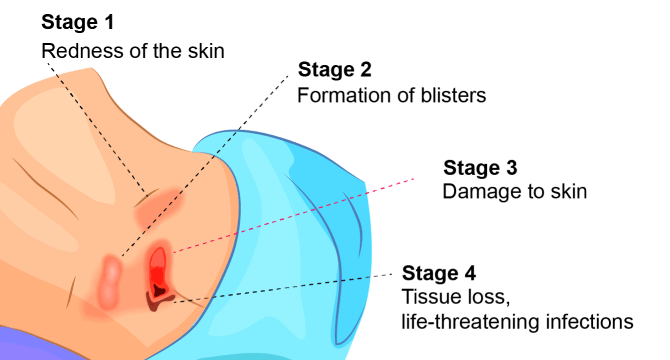
Image above shows the different stages of bedsores.
Stage 1
Stage 1 pressure sores are the easiest to treat as the skin is still intact. These nursing home bedsores usually appear as red-colored marks on the body. Stage 1 bedsores may be painful, warm, tender, and firm when compared to normal skin.
Stage 2
A stage 2 bedsore has pierced the epidermis (outer layer of the skin) and the dermis (second layer of skin). There may be a shallow wound that is red or pinkish in color, which may resemble a ruptured blister.
Stage 3
Stage 3 bedsores are deep wounds that expose fatty tissue. The ulcer typically resembles a crater with a yellow-colored base. The damage from a stage 3 bedsore may also spread to surrounding areas of normal skin.
Stage 4
Stage 4 bedsores are the most severe of all stages. Here, there is a great deal of lost tissue that can expose the tendons, muscles, or bones. The base of the wound contains dead tissue that is crusty and dark in color, and the damage extends into healthy tissue.
Get a free case review to pursue justice if your loved one suffered from a nursing home bedsore.
Possible Complications From Bedsores
While a nursing home bedsore is very dangerous in and of itself, it can also lead to additional health problems without prompt treatment.
Complications related to bedsores include:
- Cancer: Some bedsores that do not heal and become open wounds can cause a cancer called squamous cell carcinoma.
- Infections: A bedsore is usually an open wound, so bacteria can easily enter the body through it. Common infections include cellulitis (skin infection) and osteomyelitis (bone infections). Infections related to bedsores can cause brain fog, fatigue, and a rapid heartbeat, according to Johns Hopkins University.
- Sepsis: Sepsis occurs when the body’s immune system overreacts to an infection, killing healthy tissues and organs. It can even lead to a more severe condition called septic shock, which can be fatal.
Treatment for Bedsores in Nursing Homes


If you or a loved one has developed a nursing home bedsore, it needs to be treated immediately. Bedsores can worsen very quickly without treatment — but with proper care, a full recovery may be possible.
Bedsores that have broken through the skin will likely need to be treated at a medical facility. There, doctors can use proper wound care techniques to start the healing process.
To treat bedsores, doctors will:
Keep the Wound Clean
It is necessary to prevent infections by keeping any open wounds clean. If the skin has not yet broken, it should be washed with soap and water and kept dry. Open sores are often cleaned using water or saline with each dressing change.
Remove Damaged Tissue
Dead tissue must be removed through a process called debridement. If the dead tissue is not removed, it can take longer for the bedsore to heal.
Dress the Wound
Various dressings (coverings) can be used to create a barrier between areas of infection and the clean wound. These include gauze, medical gels, or bandages.
Perform Surgery if Needed
If the sore doesn’t heal by nonsurgical means, then doctors may recommend surgery. Doctors can surgically extract a patch of healthy tissue from elsewhere on the body to cover the sore. In very severe cases, limb amputation may be needed.
Stage 1 or stage 2 bedsores usually heal within a few weeks or months with proper wound care. Stage 3 and stage 4 bedsores will need more time to heal — sometimes months or years. Sadly, some severe nursing home bedsores will never heal even with treatment.
Tips for Preventing Nursing Home Bedsores


While medical care is essential to treating a nursing home bedsore, it’s equally important to prevent these ulcers before they start.
Some ways to reduce the chance of bedsores include:
Frequently Repositioning
Regular repositioning is required to prevent and treat nursing home bedsores. For wheelchair-bound individuals, weight must be shifted about every fifteen minutes.
Making Use of Support Surfaces
People with bedsores need special beds and mattresses that allow the patient to lie with the least amount of pressure.
Patients can also use a support bar in bed in order to move without having too much friction or shear. For those in wheelchairs, there are several types of wheelchair cushions that lessen the chance of bedsores.
Getting Proper Nutrition and Hydration
Eating right, getting plenty of vitamins, and staying hydrated keeps the skin healthy. Nutrition and hydration also play a big role in recovering from a bedsore.
Choosing a High-Quality Nursing Home
Before moving into a nursing home, make sure that it has a high-quality rating. See if former residents have complained about nursing home bedsores or other injuries in the past.
Remember, nursing home staff members are trained to prevent bedsores — if they fail to do so, they may be committing abuse or neglect.
How to Report Nursing Home Abuse Bedsores
If you believe a bedsore was caused by nursing home abuse, take action by reporting it. Filing a report can get your loved one the help they need and may allow you to hold the nursing home and its staff accountable.
You can report nursing home bedsores to:
- Adult Protective Services (APS)
This advocacy group investigates complaints of elder mistreatment and works to keep older adults safe. Every state has an APS branch that can be contacted to file complaints.
- Doctors
Doctors can see how severe the bedsore is and start treating it. They may also note how a bedsore may have stemmed from neglect.
- Nursing Home Ombudsmen
A nursing home ombudsman advocates for the rights of residents in nursing homes. An ombudsman can help address any concerns about the quality of care and work to resolve them.
- Nursing Home Abuse Lawyers
Personal injury lawyers that specialize in nursing home abuse cases can help you file a legal claim and pursue financial compensation.
Get Compensation for Nursing Home Abuse Bedsores
Assisted living facilities are supposed to keep older adults safe. Sadly, residents continue to develop life-threatening bedsores every year due to nursing home neglect or even abuse.
Thankfully, you and your family members can seek justice and compensation after a nursing home bedsore develops.
Don’t wait: get a free case review to see if you can work with a law firm and pursue compensation.
A skilled nursing home abuse law firm can build a claim and work to get a financial payout from a long-term care facility.
Financial compensation can cover:
- Costs of moving your loved one to a safer facility
- Medical expenses
- Pain and suffering
Common Questions About Nursing Home Bedsores
Why do nursing home residents get bedsores?
Nursing home residents get bedsores for a couple of different reasons. First, many residents have physical health problems that prevent them from moving. They may sit or lie in the same spot for too long, which cuts off blood flow to the skin.
Further, older adults may develop bedsores if a nursing home does not provide proper care. Even if a nursing home resident cannot move, a bedsore can still be prevented if staff members regularly reposition them.
Nursing homes and their staff are supposed to keep residents safe from bedsores and other health problems. If an older person you love developed a bedsore in a nursing home, it may be due to abuse or neglect.
Can you sue a nursing home for bedsores?
Yes — It may be possible to file a lawsuit for a nursing home bedsore. By filing a lawsuit, you can pursue financial compensation and justice for the harm done. Contact our team to see if you qualify.
How much is a bedsore lawsuit worth?
Nursing home bedsore lawsuits award different amounts depending on the unique factors in each case. That said, some cases have awarded millions of dollars.
In 2016, the family of a woman who died from a bedsore she developed in a nursing home received $1 million. The family claimed in their lawsuit that nursing home staff failed to properly treat the woman’s bedsore until it was too late.


