What Are Stage 3 Bedsores?
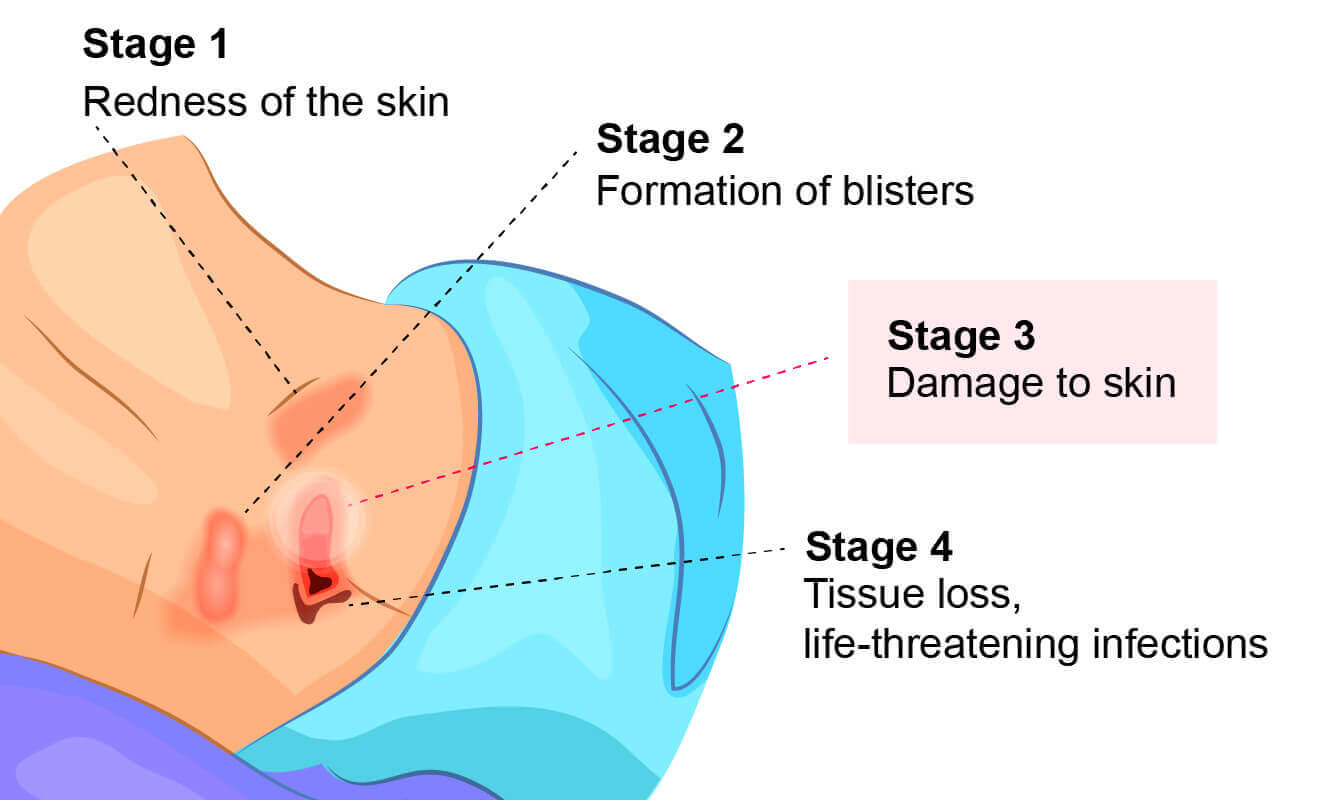
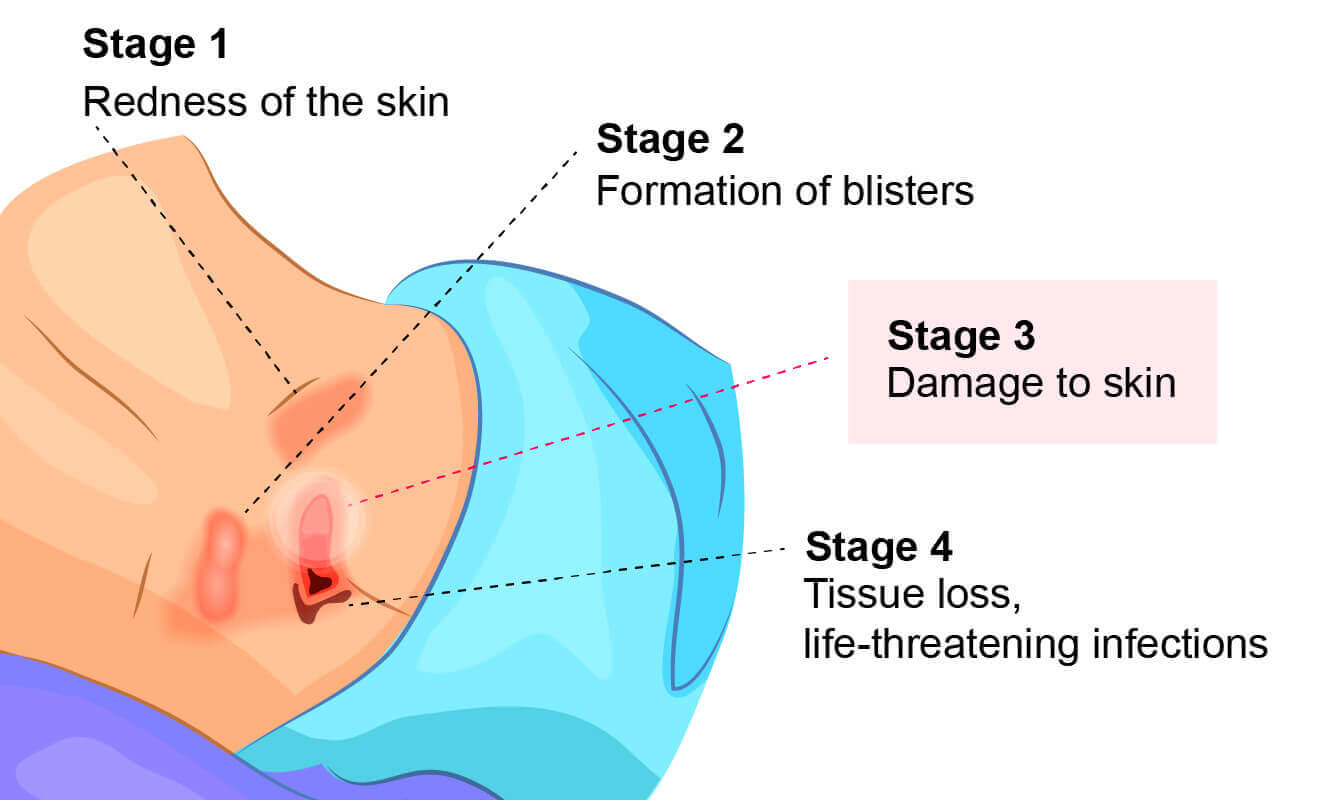
Bedsores, also known as pressure ulcers or decubitus ulcers, are broken down into four stages based on their severity. Stage 3 bedsores have burrowed past the dermis (the skin’s second layer) and reached the subcutaneous tissue (fat layers) beneath.
Stage 3 bedsores pose a high risk of infection and can take months to heal from. Some pressure sores may even progress to the fourth and most dangerous stage without proper treatment.
Nursing homes that hire enough well-trained staff can often provide the care needed to prevent serious bedsores. If a nursing home resident develops a stage 3 bedsore, it may mean the facility is not properly caring for them.
Thankfully, there are ways to get help if your loved one develops a stage 3 bedsore. For example, loved ones can access medical care to keep a resident’s bedsore from worsening. They may also be able to take legal action against the nursing home to get compensation for treatment costs.
Causes of Stage 3 Bedsores
Bedsores form when blood flow to the skin is cut off, causing healthy tissue to die and an abrasion (open wound) to appear. The longer the bedsore is left untreated, the deeper the wound may become.
Stage 3 bedsores occur when stage 2 bedsores fail to heal and the sore deepens into the patient’s skin.


Nursing home residents are at risk of bedsores if they sit or lie in the same position for long spans of time, which restricts blood flow and causes skin cells to die. While all nursing home residents with limited mobility may be vulnerable to advanced-stage bedsores, some residents have an especially high risk.
Residents are at higher risk of a stage 3 bedsore if they have:
- A cast on
- Circulation problems
- Diabetes
- Health issues stemming from malnutrition
- Spinal cord injuries that limit movement
However, stage 3 bedsores can usually be prevented even in high-risk patients. It’s the duty of nursing home staff members to identify these risk factors in patients and treat them.
Nursing Home Neglect and Stage 3 Bedsores
When a lack of care causes a resident to develop a stage 3 bedsore, nursing home neglect may have occurred.
Neglect is not the same thing as making a simple, harmless mistake — it’s a life-threatening error or series of errors. Sadly, poorly trained or inattentive staff can provide consistently poor care to residents, which can lead to bedsores.
Nursing home neglect often goes hand-in-hand with another issue: understaffing in long-term care facilities. When there are less staff members available, residents may have to wait long hours before their health care needs are addressed.
In chronically understaffed nursing homes, care problems can go unresolved for months — making it more likely for bedsores to develop.
Understaffing may lead to stage 3 bedsores, as caretakers are:
- Less likely to notice or treat bedsores in their early stages
- At a greater risk of forgetting to care for every resident
- More likely to leave a resident in bed or a wheelchair for too long
Get a free case review to get justice.
Symptoms of Stage 3 Bedsores
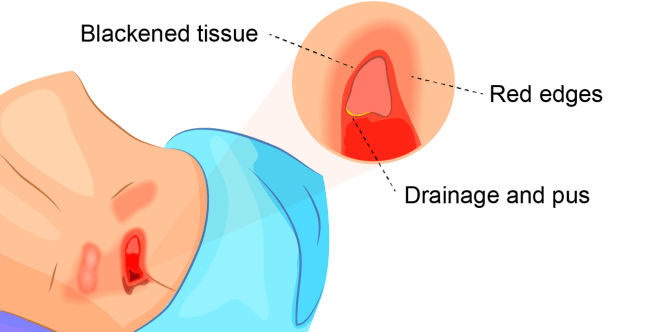
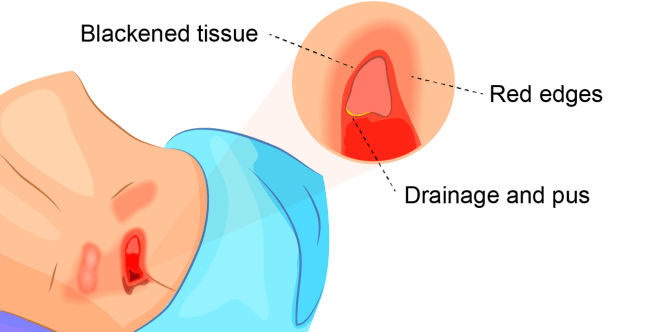
Symptoms of stage 3 bedsores include:
- Bad odor coming from the sore
- Black tissue in or around the sore
- Fever
- Green drainage and/or pus
- Redness around the sore’s edges
Several of these symptoms, including fever, drainage, and redness around the sore, are signs of infection. Because bedsores are open wounds, infections can easily set in, inviting bacteria into the body and causing complications in the healing process.
Diagnosing a Stage 3 Bedsore
A medical professional relies on a bedsore’s appearance to diagnose its stage.
Stage 3 bedsores have the following characteristics:
- Black or rotten outer edges
- Crater-like indentation
- Dead, yellowish tissue
- Visible fat tissues
Stage 3 bedsores are quite deep, but tendons, ligaments, muscles, and/or bones will not be visible. If they are, the patient likely has a stage 4 bedsore. That said, health care providers may not be able to properly stage every severe bedsore.
Two complications may delay a stage 3 bedsore diagnosis:
- Deep tissue injuries: A deep tissue injury occurs when there is no open wound but the tissues beneath a patient’s skin are damaged.
- Unstageable injuries: If a doctor cannot see the base of the sore due to slough (dead tissue) or eschar (scabs) in the wound bed, they cannot make a diagnosis.
Even if a bedsore cannot be staged, doctors can still recommend treatments to start the healing process.
Stage 3 Bedsore Prognosis
A prognosis is an expected health outcome of a disease. The prognosis for a stage 3 bedsore is worse than the lower stages but still fairly decent — they typically take 1-4 months to heal.
However, stage 3 bedsores can be life-threatening. If left untreated, stage 3 bedsores may progress to stage 4 bedsores, reaching ligaments and exposing bone. Infections associated with bedsores can even trigger a condition called sepsis, which can be fatal.
Doctors can provide a more accurate prognosis based on the specifics in each patient’s case.
Treating Stage 3 Bedsores
Wound care is essential to start the healing process for a pressure injury. Those with stage 3 bedsores should go to a doctor right away for treatments.
Treatment of stage 3 bedsores may include:
- Antibiotics to fight infection
- A special bed or mattress to help with recovery
- Debridement — the surgical removal of dead tissue
- Taking pressure off of the bedsore
Treating these injuries can be difficult because deep sores often require surgery and heal slowly. That said, it’s important to seek treatments because the alternatives — a risk of stage 4 bedsores or life-threatening infections — are much worse.
Preventing Stage 3 Bedsores
Stage 3 pressure ulcers can usually be prevented by treating earlier-stage bedsores. When an older adult lives in a nursing home, staff members are responsible for preventing bedsores and likely have protocol in place to do so.


Nursing home staff and caregivers can help prevent bedsores by:
- Keeping residents mobile
- Making sure residents are well-fed and hydrated
- Regularly repositioning residents with mobility issues
- Treating early stage bedsores as soon as possible
- Contacting a doctor if a bedsore does not heal quickly
Family members can also play a key role in preventing bedsores among nursing home residents. For example, loved ones can regularly check up on the resident and note their overall physical health.
Those who discover bedsores on their elderly loved one should speak to facility staff or a local long-term care ombudsman to make sure it’s addressed. Remember, nursing home staff are trained to keep residents safe from bedsores — not to make them worse.
Family members who are concerned about their loved one’s health can contact doctors to make sure the resident gets properly cared for. If a nursing home resident has suffered severe injuries from a bedsore, loved ones may need to work with law enforcement or lawyers to get justice.
Legal Compensation for Stage 3 Bedsores


Stage 3 pressure sores, like many nursing home injuries, are largely preventable with proper care. If your loved one developed severe bedsores in a nursing home, it may be the result of nursing home abuse or neglect.
Fortunately, you may be entitled to compensation for your pain and suffering. Get a free case review today and speak with a trusted legal partner.


