More than 1.5 million Americans reside in about 16,000 nursing facilities in the United States, as indicated by the 2004 National Nursing Home Survey.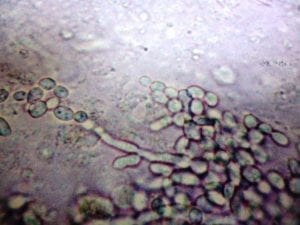
More than 88 percent of these individuals are over the age of 65 and 45 percent are greater than 85 years of age. This number is expected to reach 5.3 million people by the year 2030.
Patients in this population have become sicker over the years and it is estimated that 2 million infections occur in U.S. nursing facilities each year.
Risk factors for infections in the elderly include having indwelling devices, a recent hospital admission, impairments in function, and multiple other illnesses. As an example, residents with feeding tubes are at risk for aspiration pneumonia, skin and soft tissue infections, and other mechanical complications.
Infections and the use of antibiotics are key reasons for the presence of antibiotic-resistant organisms in the nursing home. Common organisms of this classification include methicillin-resistant Staphylococcus aureus (MRSA), resistant Gram-negative bacilli, and vancomycin-resistant enterococci.
Nursing home residents who come from hospitals or are transferred to another nursing home serve as carriers of disease, frequently introducing resistant organisms at their new places of residence.
Risk factors for having resistant organisms include old age, long-term institutionalization, functional status problems, prior antibiotic use, the presence of an indwelling device, and other illnesses.
If you or a loved one suffered a serious infection while in a nursing home, get a free case review. Compensation may be available.
Common Infections in Nursing Homes
The most common infections among nursing home residents include:
- Gastroenteritis
- Influenza
- Respiratory infections
- Skin infections
- Soft-tissue infections
- Urinary tract infections
It is impossible to provide precise estimates as to the prevalence and incidence of these types of infections in nursing homes, as there is a great deal of diversity among those infected and the way they are treated. In the 2004 Nursing Home Survey, the rate of pneumonia was 2.3 percent and the rate of UTIs was 5.7 percent among nursing home residents.
Pneumonia
Pneumonia and related lower respiratory tract infections are the leading cause of death among nursing home residents. This is also a big reason behind transfers to the hospital.
The incidence of nursing home pneumonia is about 0.3-2.3 episodes per 1,000 resident care days. Residents with feeding tubes carried the highest risk of pneumonia.
Nursing home residents in the U.S. account for 10-18 percent of all people hospitalized for pneumonia, costing about $10,000 per hospital admission.
Pneumonia in the elderly can manifest itself with some atypical symptoms that may challenge the diagnosis of pneumonia in the nursing home setting.
About a quarter of older adults may not develop a fever and are less likely to have chills, pleuritic chest pain, and muscle pain when compared to younger patients. The diagnosis is usually made by blood testing and chest x-rays.
Outbreaks of the seasonal flu are frequently reported. Influenza has been reported among staff members and residents alike who, despite getting flu shots, do not always have the proper preventative care to resist getting influenza.
Nevertheless, it is a good idea to immunize both staff members and residents against influenza. This can also reduce the death rate of older adults if their healthcare workers have also been immunized. Medications can be given to actively fight the flu if provided in a timely fashion.
Aspiration pneumonia is common among the nursing home population and is usually related to difficulties in feeding and regurgitation of gastric contents. Poor oral hygiene also significantly increases the risk of pneumonia. Dental plaque has been looked at as a source of bacteria that later causes pneumonia.
One study showed that 58 percent of nursing home residents had extensive dental needs and 30 percent reported a significant impact of their oral health on their quality of life. These studies highlight the need to provide good oral care to nursing home residents.
Urinary Tract Infections
The UTI is perhaps the most common infection in the nursing home and is the most over-diagnosed infection among nursing home residents. The presence of an indwelling catheter increases the risk of bladder infections and bacterial sepsis from urinary tract organisms.
About 3-7 percent of nursing home residents with an indwelling catheter will get a urinary tract infection with each day that the catheter remains in place. By the 30th day, about 100 percent of residents will have bacteria in the urine.
Half of all nursing home residents will have symptomatic urinary tract infections. The mortality rate for those who have indwelling catheters is higher than for those who do not have a catheter.
Diarrheal Diseases
Bacterial and viral gastroenteritis is the cause of the majority of attacks of diarrhea in the nursing home. Older adults do not produce enough gastric acid and are at a greater risk of developing infectious gastroenteritis.
Usually, the clinical course of these infections is self-limited and no treatment is recommended. Gastroenteritis can be associated with an increase in morbidity and mortality, mainly because these are people who have a greater risk of dehydration.
Studies have shown that nursing home residents are four times more likely to die from gastroenteritis than those older adults residing in the community.
Norovirus remains a common cause of dehydration and gastroenteritis in nursing home residents and is responsible for half of all gastroenteritis outbreaks throughout the world. It has been estimated that about 21 million cases of norovirus occur each year in the U.S. alone.
Norovirus is a very contagious virus and can be transmitted from person to person, and through food and water as well. Nursing homes are frequent sites for outbreaks of these kinds of viruses. About 35 percent of norovirus outbreaks reported by the CDC occur from nursing homes.
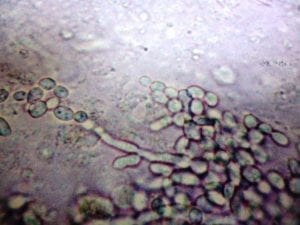
Clostridium difficile infections are an emerging cause of infectious diarrhea among nursing home residents. The incidence of colonization in nursing homes varies from 4 to 20 percent.
About 8-33 percent of nursing home residents treated with antibiotics will get a secondary infection with Clostridium difficile. About 10-30 percent of nursing home residents are colonized with the organism at any given time.
See if you can get compensation for serious infections with a free case review.
Skin and Soft Tissue Infections
Older nursing home residents are especially predisposed to getting skin and soft tissue infections due to the various changes in the skin as a result of aging.
This includes the atrophy of the dermis and epidermis, decreased resistance to external insults, and prolonged wound healing times. Dry, itchy skin can serve as an entry point for bacteria that can infect the skin.
Typical nursing home skin infections include cellulitis, necrotizing fasciitis, and erysipelas. Chronic wound infections are more common, including infected pressure ulcers, vascular ulcers, and diabetic wound infections. Other types of skin infections include intertrigo, tenia versicolor, herpes zoster, scabies, and herpes simplex.
Pressure ulcers in nursing homes are a frequent phenomenon. Risk factors include immobility, impaired mental capacity, incontinence, impaired nutrition, and a greater degree of other illnesses. Older adults who are frail are at a higher risk of developing pressure ulcers and having these pressure ulcers become infected.
The infections can lead to additional infections in the bone, skin, blood and can result in death. This is why these infections need to be prevented, recognized early, and treated correctly.
Get a free case review today to see if you or your family qualifies for financial compensation after an infection.


