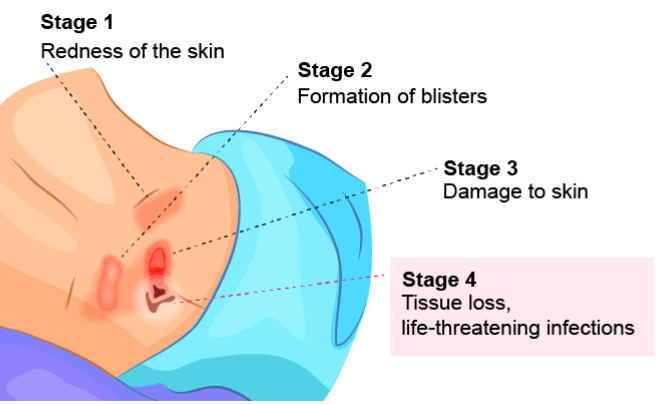
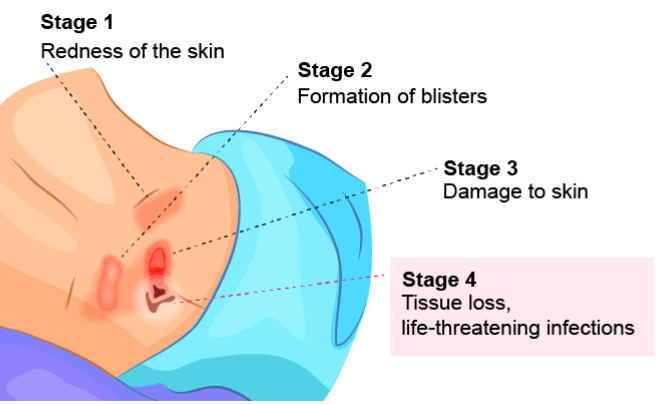
What Is a Stage 4 Bedsore?


A stage 4 bedsore is a deep wound reaching the muscles, ligaments, or bones. It is the most severe form of a bedsore (also called a bed sore, pressure sore, pressure ulcer, or decubitus ulcer.)
Bed sores stage 4 are the worst-case scenario: the blood supply has been so severely cut off that the wound tunnels down through all layers of the skin and exposes bone. They often cause extreme pain, infection, and even death. Many residents must undergo invasive surgeries to survive stage 4 bedsores.
Sadly, a stage 4 pressure ulcer is often a sign of nursing home neglect. Residents of nursing homes may develop these sores if caregivers fail to treat earlier pressure ulcer stages. A stage 4 pressure ulcer usually means a nursing home resident has stayed in the same position for an extended period of time.
Thankfully, financial compensation may be available if your loved one developed bed sores stage 4 while living in a nursing home.
Get a free case review now to see if you can pursue compensation.
What Does a Stage 4 Bedsore Look Like?
A stage 4 bedsore is the largest and deepest of all bedsore stages. Characterized by severe tissue damage, a stage 4 pressure ulcer may look like a reddish crater on the skin.
Muscles, bones, and/or tendons may also be visible at the bottom of the stage 4 pressure ulcer.
When infected, bed sores stage 4 may have a foul smell and leak pus. Additionally, the sore may be surrounded by dead tissue that’s dark or yellowish in color.
Stage 4 Bedsore Causes
Bed sores stage 4 are caused by factors like pressure, shear, and friction that cut off the blood supply to the skin. Without proper treatment, this loss of blood flow can cause the skin to die and a wound to form, eventually turning into a stage 4 bedsore.
“Being bedridden, unconscious, unable to sense pain, or immobile increases the risk that a bedsore will develop. The risk increases if the person is not turned, positioned correctly, or provided with proper nutrition and skin care.”
—Johns Hopkins Medicine
Therefore, in nursing homes, bed sores stage 4 are usually the result of improper care from staff. This is especially true for advanced cases, which can form if earlier-stage pressure injuries are not properly treated.
Nursing home residents may develop bedsores if staff members:
- Cannot adequately care for each resident due to understaffing
- Don’t treat dehydration or malnutrition, which can prevent healing or worsen sores
- Fail to notice or treat earlier-stage sores due to skipped or rushed care
- Leave residents with mobility issues lying in beds or wheelchairs for hours on end
Who’s at Risk of Developing a Stage 4 Pressure Ulcer?
Anyone with a lower-stage bedsore is at risk of developing bed sores stage 4 if the wound is not treated. However, some patients may have other health conditions making them more prone to this type of injury.
At particularly high risk for stage 4 bedsores are people who:
Have Limited Mobility
According to the National Pressure Ulcer Advisory Panel (NPUAP), “a number of contributing or compounding factors are associated with pressure injuries; the primary of which is impaired mobility.” Movement is the key to preventing bedsores at any stage.
If nursing home residents cannot move on their own, they may sit or lie in the same position for hours. This can cut off blood flow to their skin and cause a bedsore. Once a bedsore forms in a person with limited mobility, it can quickly advance to a stage 4 pressure ulcer.
Live in Understaffed Nursing Homes
Nursing home residents with mobility issues must rely on staff members to prevent bedsores. Sadly, some care facilities may fail to prevent bedsores due to nursing home understaffing and poor training. In these cases, nursing home neglect is almost always at play.
Have Alzheimer’s or Dementia
If residents with cognitive impairments develop a bedsore, they might be unable to tell anyone due to their condition. They’ll need to have someone else find it and help them get proper care.
According to the Alzheimer’s Society, “It is important for anyone caring for a person with dementia to know about pressure ulcers.”
Residents with these conditions may also have trouble sensing pain. This means a bedsore may go unnoticed before it advances to a stage 4 pressure ulcer.
Other Factors
Nursing home residents are at higher risk of developing a stage 4 pressure ulcer if they have blood flow or circulation problems that require diabetic care or if they wear a cast.
Can You Sue for a Stage 4 Bedsore?
Yes. You may be able to file a lawsuit for a stage 4 bedsore. If a nursing home or other care facility fails to protect residents from harm, victims and their loved ones can sue for nursing home neglect.
This is because a stage 4 pressure ulcer that was allowed to progress through all the other stages into its most severe and final stage (bed sores stage 4) is likely to be a sign of neglect.
In 2022, a jury awarded over $10 million to a Florida nursing home resident who developed a stage 4 pressure injury that required surgery. Learn more about nursing home lawsuit compensation now.
Remember: Bedsores are almost always preventable. A care facility must monitor for signs of pressure injuries and take preventative measures so they do not worsen.
When a wound becomes a stage 4 pressure ulcer, it can be excruciating and cause great suffering. It can even lead to death.
A skilled personal injury lawyer specializing in nursing home abuse or neglect can help you understand your legal rights. Get started now by finding out if you can file a stage 4 bedsore lawsuit.
Symptoms of a Stage 4 Pressure Ulcer
Most symptoms of bed sores stage 4 are related to bacterial infections in nursing homes, a common complication. This is because bacteria can easily enter the body through open sores, such as a severe bed sore.
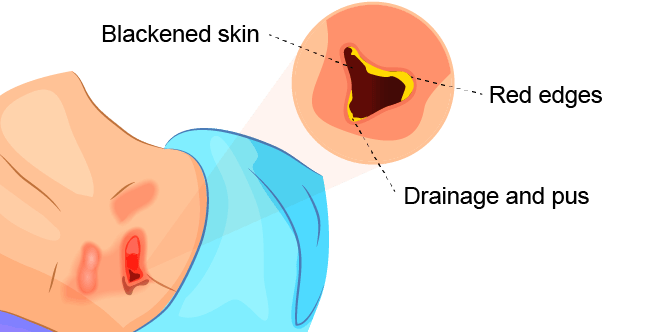
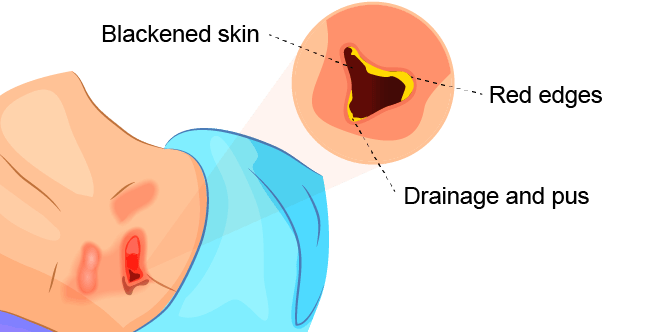
Symptoms of a stage 4 bedsore include:
- Blackened or darker skin
- Drainage and pus
- Fever
- Hot skin
- Odor
- Open wounds exposing tissue or bone
- Red edges
- Swelling around the sore
If you notice any of these stage 4 pressure ulcer symptoms in your loved one, seek immediate medical care.
You may also want to connect with a nursing home abuse lawyer to see if you can take legal action and receive financial compensation.
Diagnosing a Stage 4 Pressure Ulcer
A doctor determines the stage of a bedsore by its appearance. In the case of a stage 4 bedsore, the large wound has passed the body’s fatty tissue layer, exposing muscles, ligaments, or even bone.
In some cases, however, health care professionals may not be able to immediately diagnose a late-stage bedsore by examining it.
A stage 4 bedsore may be initially diagnosed as:
- UnstageableWhen a doctor cannot see the bottom of an open sore, they must clean it out to properly stage it.
- Suspected Deep Tissue Injury (SDTI)A diagnosis of SDTI happens when the surface of a patient’s skin looks like a stage 1 or 2 bedsore, but it is actually affecting deeper tissues underneath. Although it looks less severe, SDTIs are likely to be stage 3 or stage 4 pressure ulcers.
Stage 4 Bedsore Treatment
Stage 4 bedsores should be treated as soon as possible, as they put a nursing home patient at high risk of deadly health problems.
Stage 4 pressure ulcer treatment options may include:
-
Antibiotics
Giving patients bacteria-destroying medicine to treat infections
-
Debridement
Removing any damaged, infected, or dead tissue from the bedsore
-
Skin Grafts
Covering the affected area with healthy skin
It can take anywhere from 3 months to 2 years for bed sores stage 4 to heal, according to the Model Systems Knowledge Translation Center (MSKTC).
Can a Stage 4 Pressure Ulcer Be Prevented?
Yes. Like many nursing home injuries, late-stage bedsores (such as bed sores stage 4) are largely preventable with proper care.
They can be avoided by treating a stage 3 bedsore or lower-stage bedsores from forming in the first place.
The top 5 ways to prevent stage 4 bedsores are:
- Treating early-stage bedsores as soon as possible with proper wound care practices
- Carefully monitoring earlier-stage bedsores to ensure they are healing
- Contacting health care providers if a patient’s wound is not improving
- Keeping residents mobile by walking and repositioning them
- Making sure residents have access to regular meals, water, and skincare
Sadly, research shows many nursing homes do not report bedsores to Medicare even though they are required to by law. This can make it especially hard for negligent nursing homes to be held accountable for failing to prevent stage 4 bedsores.
“40% of bedsores in long-term residents were not reported to the Nursing Home Compare database.”
—U.S. News & World Report
This is alarming because many families rely on Medicare’s rating tools to choose a nursing home or assisted living facility for their loved ones. How can people be expected to find safe facilities for their loved ones if critical data is hidden?
It is unacceptable if your loved one developed a stage 4 bedsore while in the care of a nursing home. Find out if you can hold the facility accountable through a lawsuit with a free legal consultation now.
Complications From Stage 4 Bedsores
Those with a stage 4 bedsore are at high risk of life-threatening complications.
If left untreated, a stage 4 bedsore may lead to:
Amyloidosis
This is an incurable condition where protein builds up in the body and prevents organs from functioning properly.
Infection
According to Johns Hopkins Medicine, those with a stage 4 bedsore are at a very high risk of infections. These infections can affect the skin, bones, blood, and other organs.
For example, osteomyelitis (bone infection) and cellulitis (skin infection) can be caused by bacterial infections stemming from the stage 4 pressure ulcer.
Renal Failure
This occurs when the kidneys can no longer remove waste from the body, causing damage. It can be fatal if left untreated, but recovery may be possible.
Sepsis and Septic Shock
Sepsis may occur when the body overreacts to a serious infection, such as an infection stemming from a stage 4 bedsore. The immune system gets overstimulated and attacks a healthy part of the body.
Severe cases of sepsis can lead to septic shock, which occurs when blood pressure drops due to an infection. Septic shock can be deadly as major organs may shut down.
Death
Many of the conditions listed above can be fatal if left untreated. According to the Western Journal of Medicine, renal failure and amyloidosis are the most common causes of death for patients suffering from chronic bedsores.
Roughly 60,000 people die as a direct result of pressure ulcers every year.
It may be considered wrongful death if a nursing home resident dies after developing bed sores stage 4.
Stage 4 Bedsore Life Expectancy
The life expectancy for stage 4 bed sores depends on several different factors. If the bedsore is treated properly before signs of infection appear, it is possible to fully recover.
With proper medical care, stage 4 bedsore life expectancy is several months or years.
However, without specialized medical care, blisters that have advanced through the stages of pressure sores to stage 4 are more likely to cause complications or even death.
“Once a bedsore develops, it can take days, months, or even years to heal. It can also become infected, causing fever and chills.”
—Johns Hopkins Medicine
According to the National Institutes of Health (NIH), bedsores that lead to sepsis cause thousands of deaths per year.
The best defense is recognizing and treating pressure sores before they reach stage 4.
Stage 4 Bedsore: Get Help
When a resident of a care facility suffers from a stage 4 bedsore, it is often due to nursing home neglect. Fortunately, families have options if neglect or abuse has caused stage 4 bed sores.
Here are steps you can take if your loved one has a stage 4 bedsore:
- Seek immediate medical care by insisting they be transferred to a hospital.
- When they are released from the hospital, consider moving them to another nursing home to recover.
- Report the stage 4 bedsore to your state’s ombudsman or your local Adult Protective Services (APS).
- Connect with a top nursing home neglect law firm near you to file a legal claim and pursue compensation.
Over 17,000 lawsuits involving bedsores are filed each year. The best way to find out if you can sue for a stage 4 bedsore is to contact a nursing home abuse lawyer.
Get a free case review now to find out what options are best for your family. You may be able to file a stage 4 bedsore lawsuit to access the funds you need for your loved one’s care.
FAQs About Stage 4 Bedsores
What is most likely to cause bedsores?
Bedsores usually form on the bony areas of the body, such as the tailbone, shoulder blades, hips, heels, and ankles.
They are most likely to occur in people with a limited ability to move on their own, including people who spend most of their time in a wheelchair or lying in bed.
What is a stage 4 pressure ulcer?
A stage 4 pressure ulcer is another term that is used to describe stage 4 bed sores. Different medical professionals and care facilities may use the terms interchangeably.
However, it is important to understand that they are the same and are almost always caused by neglect, which is a form of nursing home abuse.
Can a stage 4 bedsore be prevented?
Yes. Stage 4 bedsores can be prevented with proper care. This includes repositioning and providing soft padding, adequate nutrition, and good skincare.
Treating a pressure ulcer as soon as it starts is critical, or it could quickly progress to a stage 4 bedsore.
Can bedsores cause sepsis?
Yes. Sepsis develops when the body tries too hard to fight infection. A stage 4 bedsore can trigger the infections that lead to sepsis.
A joint study from the Chicago Tribune and Kaiser Health News found that nursing homes consistently fail to treat bedsores and other conditions that lead to sepsis. In one case, a resident died after developing a serious bedsore that led to sepsis.
His daughter later filed a nursing home lawsuit, claiming his death caused by sepsis could have been prevented.
How long can you live with a stage 4 bedsore?
Patients can live for months or even years after developing a stage 4 bedsore. Factors such as proper medical care and preventing complications can help patients live longer.
That said, roughly 60,000 people die each year due to bedsore-related complications. Over 50% of those who develop bedsores in hospital settings die in a year or less, according to a 2020 study.
Can stage 4 bedsores heal?
Yes. However, it depends on when treatment is sought and other factors. According to the medical textbook Merck Manual, 30% of stage 4 bedsores will heal in six months.
Some bedsores may not properly heal — due to complications like bacterial infections — despite proper care. In these cases, doctors can check for secondary complications and treat those alongside the bedsore.
Are stage 4 bedsores always a sign of nursing home abuse?
Since bedsores can usually be prevented with proper care, they may be a sign of elder abuse or nursing home neglect. This is especially true when a bedsore is allowed to progress through the earlier stages of bedsores all the way to stage 4.
Can I sue for a stage 4 bedsore?
Yes. Stage 4 bedsores are almost always preventable. Thus, you may be able to hold the staff accountable by filing a nursing home neglect lawsuit.
The presence of stage 4 bedsores usually means warning signs were ignored in the earlier stages of bedsores. Instead of intervening, negligent nursing home staff allowed the wound to progress to this excruciatingly painful and deadly stage.


